Introduction to junctional epithelium
The term junctional epithelium denotes the tissue that is affixed to the tooth on one side and to the oral sulcular epithelium and connective tissue on the other side 17, 100. The junctional epithelium is the epithelial component of the “dentogingival unit” that is in contact with the tooth surface. It has two distinct basal laminas, the external basal lamina which is continuous with the basal lamina of the sulcular epithelium and attaches the junctional epithelium to the underlying connective tissue and the internal basal lamina that attaches the junctional epithelium to the tooth surface.
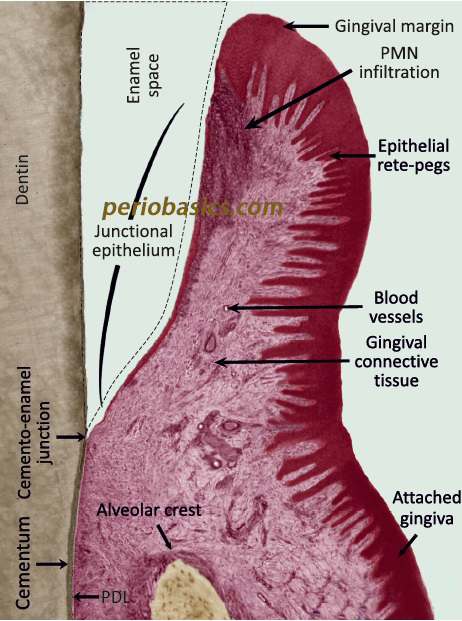
It is not keratinized on its free surface layer, so it cannot act as a physical barrier. Hence, other structural and functional characteristics of junctional epithelium must compensate for the absence of this barrier. The junctional epithelium fulfils this difficult task with its special structural framework and the collaboration of its epithelial and non-epithelial cells that provide a very potent antimicrobial mechanism. However, these defense mechanisms do not preclude the development of extensive inflammatory lesions in the gingiva. The conversion of junctional epithelium to pocket epithelium is regarded as the hallmark in the progression of gingivitis to periodontitis. That is why it is a dynamic structural entity and its structure and function differs significantly from the oral gingival epithelium. General and microscopic features of junctional epithelium:
- Its thickness varies from 15-18 cells at the base of the gingival sulcus to 1-2 cells in its most apical portion.
- Cells are arranged in the base and the suprabasal layers only. The apical aspect of the junctional epithelium is the site for new cell formation from where cells migrate coronally and desquamate.
- Basal cells and adjacent 1-2 suprabasal layers of cells are cuboidal or slightly spindle-shaped. All remaining cells of the suprabasal layer are flat, oriented parallel to the tooth surface and closely resemble each other. The rate of cell desquamation in the junctional epithelium is greater than that observed in the sulcular epithelium, suggesting its high turnover rate.
- The innermost layer of suprabasal cells (facing the tooth surface) are called DAT cells (directly attached to the tooth) 101.
- Lysosomal bodies are found in large numbers in the junctional epithelial cells. The enzymes contained within these lysosomes participate in the eradication of bacteria 102.
- Junctional epithelial cells have numerous Golgi apparatus, abundant rough endoplasmic reticulum with cisternae and polyribosomes.
- As already stated, junctional epithelial cells exhibit a unique set of cytokeratins including cytokeratin 5, 13, 14 and 19. Occasionally, the weak activity of cytokeratins 8, 16 and 18 is also seen 103. As compared to other epithelia, junctional epithelial cells are interconnected by a few desmosomes and occasionally by gap junctions 46, 104-106. These features account for the remarkable permeability of the junctional epithelium.
- A variety of mononuclear leukocytes occupy these interstitial spaces. Neutrophils (PMN’s) are found in the central region of the junctional epithelium and near the tooth surface 50.
- These mononuclear cells along with their products, products of junctional epithelial cells, blood and tissue fluid represent the first line of defense in the control of the perpetual microbial challenge. These molecules include α- and β-defensins, cathelicidin LL-37, interleukin-8 (IL- 8), IL-1 α and -1 β, tumor necrosis factor- α, intercellular adhesion molecule-1, and lymphocyte function antigen- 3.
- Antigen-presenting cells (APC’s), Langerhan’s cells and other dendritic cells are present as well 107.
- Junctional epithelium, particularly its basal cell layers are well innervated by sensory nerve fibers 108-111.
- In the absence of clinical signs of inflammation, approximately 30,000 PMN’s migrate per minute from the junctional epithelium of all teeth into the oral cavity 112.
- Cells originate in the basal layer and migrate in an oblique direction towards and along the tooth surface, where they are sloughed from the free surface.
- Junctional epithelial cells show no signs of synthesis of membrane coating granules, a finding that agrees with the fact that the junctional epithelium is highly permeable to water soluble substances. The chief barrier to the passage of substances larger than 100 KDa is provided by the external basal lamina.
Formation of junctional epithelium
To understand the formation of junctional epithelium, first, we must understand the development of epithelium-tooth interface. The following concepts have been proposed historically to explain the development of epithelium-tooth interface.
Gottlieb’s concept
Gottlieb’s experimental and clinical observations led to the concept that the soft tissue of gingiva is organically united to enamel surface 113, 114. He termed the epithelium contacting the tooth surface along with the interface substance as the “epithelial attachment”. According to this concept, after the completion of enamel matrix formation, the ameloblasts finally produce “primary enamel cuticle” 115. This layer is continuous with the enamel matrix and attaches the cells of REE (reduced enamel epithelium) to the calcified tooth structure.
With the eruption of the tooth, the reduced enamel epithelial cells unite with proliferating oral epithelium. As a result, the epithelial cells adjacent to the enamel surface produce a cornified layer. Gottlieb called this layer as “secondary enamel cuticle”. This layer subsequently becomes separated from the tooth surface, leaving a V-shaped groove, the gingival crevice.
Orban’s concept
Orban and his colleagues gradually modified Gottlieb’s concept in 1944. Orban (1949) 116 incorporated the views of Mayer 117, 118, Beck 119, 120 and Weski 121 and proposed that the separation of the epithelial attachment cells from the tooth surface involved preparatory degenerative changes in the epithelium 116. This concept was contradictory to the earlier concept proposed by Gottlieb, which suggested the production of a cornified cuticle layer. Waerhaugh’s concept Until 1952, the Gottlieb’s concept of epithelial attachment was quite popular in spite of objections raised against it. In 1952, Waerhaugh presented the concept of “epithelial cuff” 122. This concept was based on the observations made by insertion of thin blades between the surface of the tooth and gingiva. The blades could be passed apically to the connective tissue attachment at the CEJ without resistance. Based on these findings and other microscopic findings, he concluded that the gingival tissue and tooth are closely adapted but not organically united.
Schroeder and Listgarten’s concept
Resolution of the controversy regarding the nature of the epithelial-tooth interface was not possible until the introduction of transmission electron microscope. In their extensive studies, Schroeder and Listgarten illustrated the details of the structural relationship of epithelial tooth interface 123. They proposed the following terminologies, Primary epithelial attachment is the term that has been used to describe the relationship of……………….Content available in the hard-copy of the website……………… Content available in the hard-copy of the website…………..
Periobasics A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Junctional epithelial attachment at molecular level
The junctional epithelium is an important component of the attachment apparatus facing both the gingival connective tissue and tooth surface. The basement membrane is interposed between the basal cells of the junctional epithelium and gingival connective tissue. Basal lamina forms a part of the interfacial matrix between the tooth facing junctional epithelial cells and tooth surface (DAT cells). At the apical end of the junctional epithelium, basal lamina and basement membrane are continuous.
Basement membrane
The basement membrane is a thin membranous layer of connective tissue that separates the layer of epithelial cells from the underlying lamina propria. It is an important structural entity which is crucial for compartmentalization (physical barrier function), filtration (selective permeability barrier function), migration, cell polarization, adhesion, and differentiation. Under an electron microscope after heavy metal staining, the basement membrane consists of an electrodense part, lamina densa, and an electoleucent part, lamina lucida. The width of basal lamina is reported to be in the vicinity of 800 A˚-1200 A˚.
The immunostaining reveals that the basement membrane is composed of collagen Type IV, laminin, heparan sulfate proteoglycan, entactin, and fibronectin. The basement membrane of junctional epithelium resembles other basement membranes, but basal lamina has distinctly different structural and molecular characteristics. It lacks most of the common basement membrane components such as collagen Type IV and VII, most laminin isoforms, perlecans and a lamina fibroreticularis 125-127.Thus, basal lamina of junctional epithelium has its own characteristic features and cannot be regarded as the basement membrane in the true sense.
Expression and functions of molecular factors associated with junctional epithelial cells
The cell-matrix and cell-cell interactions are mediated by various cellular receptors. In the cellular cytoplasm, these receptors are frequently associated with signaling molecules that respond to the binding of extracellular ligands. Junctional epithelium cells express numerous cell adhesion molecules (CAM’s), such as integrins and cadherins 128. These molecules play an important role during the inflammatory response, facilitating the migration of various cells, which participate in the inflammatory response such as PMN’s, monocytes etc. Following is the general facts about the molecular factors associated with junctional epithelium.
- Integrins are cell surface receptors that mediate interactions between the cell and extracellular matrix, and also contribute in the cell to cell adhesion 129, 130. The expression of integrins is highest in the basal cell layer.
- Cadherins are responsible for the tight contacts between cells 128, 131. E-cadherin, an epithelium-specific cell adhesion molecule, plays a crucial role in maintaining the structural integrity of the junctional epithelium.
- Intercellular adhesion molecule-1 (ICAM-1 or CD-54) on the cellular surface attaches to its ligand lymphocytic function antigen-3 (LFA-3), facilitating the cellular adhesion.
- α6β4 integrin receptor is expressed by cells in contact with the internal basal lamina.
Role of intercellular adhesion molecules (ICAM’s) in immunoregulation
ICAM’s belong to the immunoglobulin receptor family, which facilitate cell-cell interactions in inflammatory reactions. They function as ligands for β2 integrin molecules present on leukocytes and participate in the control of leukocyte migration into inflammatory sites. Intercellular adhesion molecule-1 (ICAM-1) is a critical adhesion molecule for the migration of neutrophils. Expression of ICAM-1 and lymphocyte function antigen-3 (LFA-3) has been demonstrated in the junctional epithelial cells 132-135. The expression of ICAM-1 by the epithelial cells is regulated by proinflammatory cytokines such as IL-1 and TNF-α 136, 137.
The high expression of IL-8, a chemotactic cytokine by the junctional epithelial cells is a potent mechanism of PMN migration towards the bacterial challenge. It creates a chemoattractant gradient towards the bottom of the sulcus facilitating routing PMN’s to counter the invading bacteria 135, 138.
Mucosa and junctional epithelium around the dental implants
The mucosa that surrounds an oral implant is not much different from the gingiva around the teeth. Studies done on animal models have analyzed the structural characteristics of the gingiva (around teeth) and the mucosa that encompasses implants 139-144. Their observations were; the healthy, soft, keratinized tissues facing teeth and implants frequently have a pink color and a firm consistency. The two tissues have several microscopic features in common. The gingiva as well as the keratinized, peri-implant mucosa is lined by a well keratinized oral epithelium that is continuous with the junctional epithelium which is about 2 mm long. The junctional epithelium at a tooth site terminates at the CEJ, apical to which an acellular, extrinsic fiber cementum establishes, which is an important component of the supraalveolar attachment apparatus. The distance between the CEJ and the bone crest is about 1 mm and is characterized by the presence of collagen fibers that project from the cementum into the connective tissue and the bone.
Around an implant with healthy peri-implant tissue, the apical portion of the junctional epithelium is consistently separated from the alveolar bone by a zone of non-inflamed, collagen-rich but cell-poor connective tissue. In the collagen-rich zone, the fibers invest in the ……………..Content available in the hard-copy of the website……………… Content available in the hard-copy of the website…………..
Periobasics A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Regeneration of junctional epithelium
Injury to junctional epithelium may occur due to intentional or accidental trauma. Usually, it occurs due to accidental trauma during brushing, flossing or eating. Intentional trauma occurs during periodontal surgeries where the junctional epithelium is completely lost. Many studies have been done to investigate the renewal of junctional epithelium. These include studies done on the renewal of junctional epithelium on tooth and implant surface after mechanical detachment by probing, studies done on mechanical trauma during flossing and studies on regeneration of junctional epithelium after gingivectomy procedure which completely removes the junctional epithelium.
A study was done on marmosets in which probing was used to mechanically detach the junctional epithelium. A new and complete attachment, indistinguishable from that in controls was established 5 days after complete separation of the junctional epithelium from the tooth surface 148. Another study done on dental implants revealed that healing around the implants takes almost the same time for re-establishment of junctional epithelium as that around the tooth 149. Both of the above studies showed that probing injury is a completely reversible injury to the junctional epithelium.
One study investigated the healing of junctional epithelium after mechanical trauma by flossing. The results of the study revealed that detachment of cells persisted for 24 hours after cessation of flossing. New attachment of junctional epithelial cells started 3 days after cessation of flossing. After 2 weeks, the cell populations on the experimental and control surfaces were again indistinguishable from each other 150.
Many studies have been done to investigate the formation of new junctional epithelium after periodontal surgeries, as these surgeries completely remove the junctional epithelium 151-154. In a human study, that evaluated healing following an inverse bevel flap, it was demonstrated that a newly differentiated attachment apparatus with the normal hemidesmosomal attachment was formed following the surgery. This new attachment apparatus was seen on cementum as well as on dentin 152. Another study performed gingivectomies on two young cynomolgus monkeys and examined block sections of the tooth/gingiva at 12 days and 3, 4, and 7 weeks post surgery. The electron microscopic examination revealed that the junctional epithelium was completely re-established within 12 days. Hemidesmosomes appeared to form prior to the basal lamina. The basal lamina initially formed in close proximity to the hemidesmosomes at both the tooth and connective tissue interface. At 4 to 7 weeks, the basal lamina appeared to be completely formed 155. Studies have shown that regeneration of junctional epithelium after gingivectomy procedure usually occurs within 20 days 49, 155, 156.
Turnover of the attachment epithelium
One study investigated renewal time of the gingival epithelium cells in marmosets using injections of tritiated thymidine and autoradiography. Epithelial cells in the attached gingiva exhibited a renewal rate of 10.4 days, whereas the corresponding rate for the epithelial cuff was 5.8 days 157. In another study, autoradiography was used to study the rate of migration of attachment epithelium. The authors observed that the rate was comparable to the rate of tooth eruption, suggesting that the location of the attachment is relatively stable 92.
Conclusion
Junctional epithelium plays a very important role in the maintenance of periodontal health. It acts as the initiation point for the host-microbial interactions in periodontal disease progression. Hence, in-depth knowledge of the structure and function of junctional epithelium is very important to understand the etiopathogenesis of periodontal diseases.
References
References are available in the hard-copy of the website.
Periobasics A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

